Research at Costerton Biofilm Center
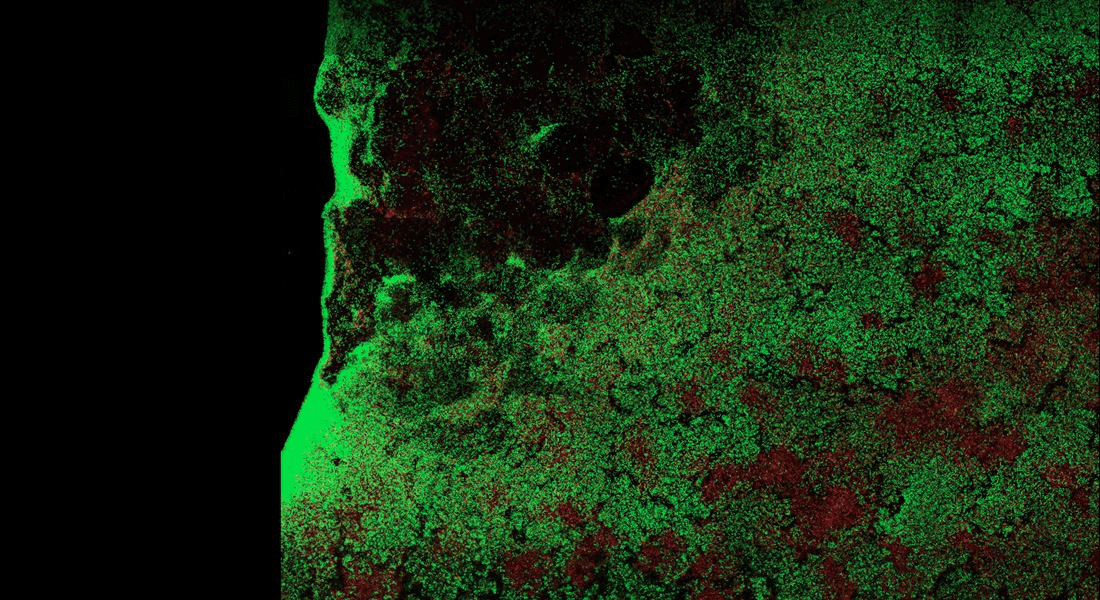
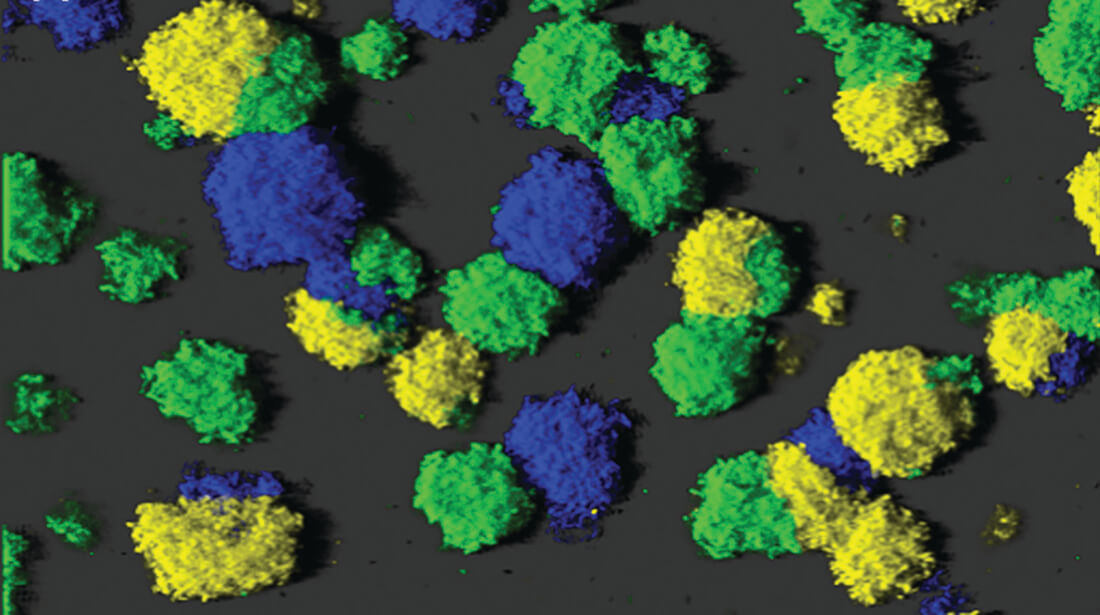
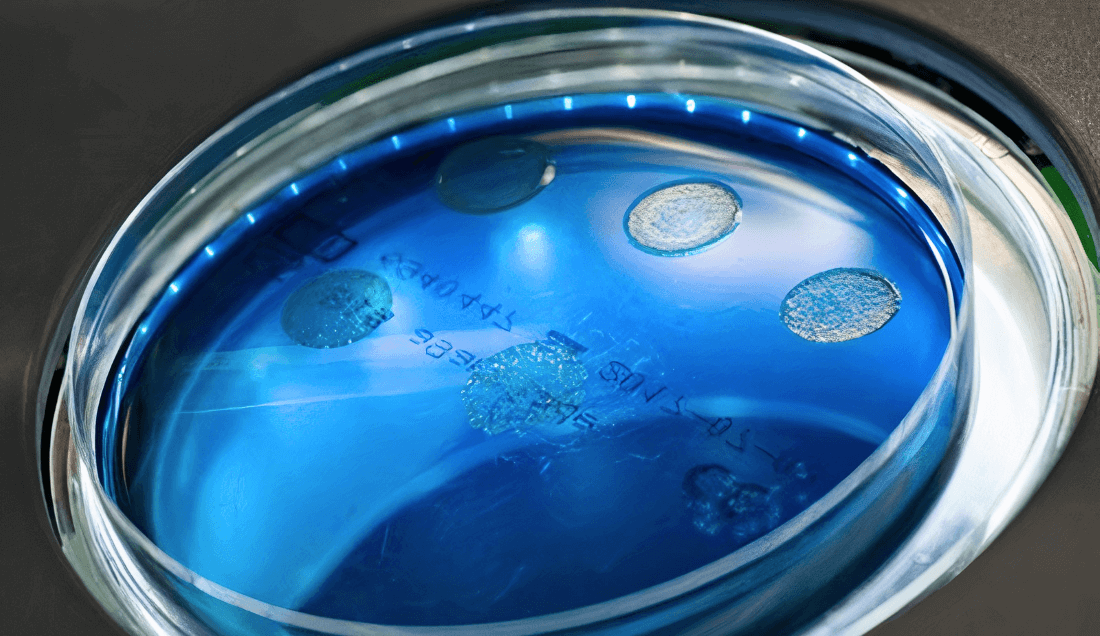
The Center provides a forum for scientists and clinicians and encourages research into the microbial aetiology of biofilms.
By integrating translational and clinically relevant research, the Costerton Biofilm Center takes lead in improved prevention and development of new treatments of diseases caused by biofilms. The research aims at explaining the riddle as to why biofilm-bacteria gain the upper hand in the fight against our immune system, and hopefully lead to new and innovative strategies for early diagnosis, treatment and prevention of chronic diseases for the benefit of public health.